A new approach to treating metastatic non-small cell lung cancer (NSCLC) published open access: TUSC2 immunogene enhances efficacy of chemoimmuno combination on KRAS/LKB1 mutant NSCLC in humanized mouse model
Although the addition of checkpoint blockade to chemotherapy as first-line treatment has improved survival in stage 4 NSCLC, the majority of patients recur after 30 months. The TUSC2 gene encapsulated in nanovesicles and injected intravenously selectively kills cancer cells and augments the anti-tumor immune response. This preclinical study showed that the addition of immunogene therapy improves the efficacy of checkpoint blockade + chemotherapy. Complete responses were observed in humanized mice with metastatic human KRAS/LKB1 mutant NSCLC.
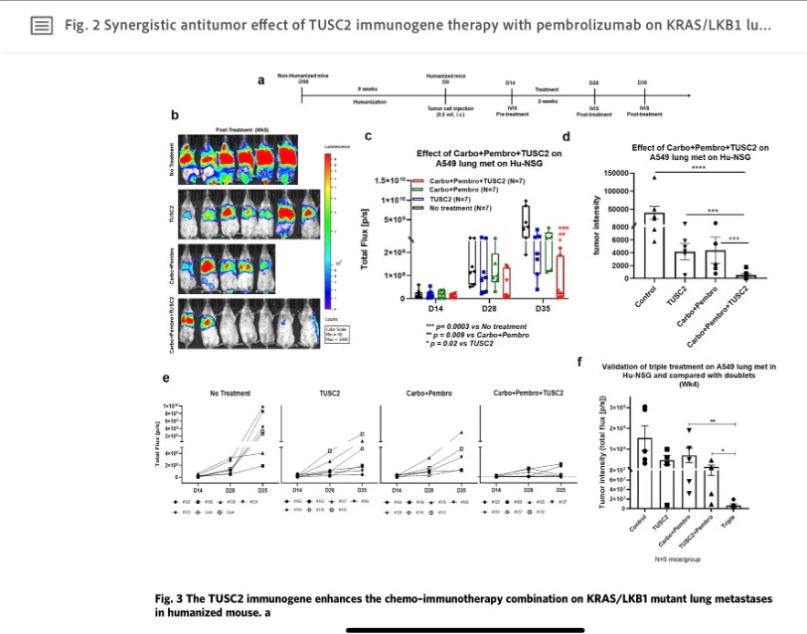
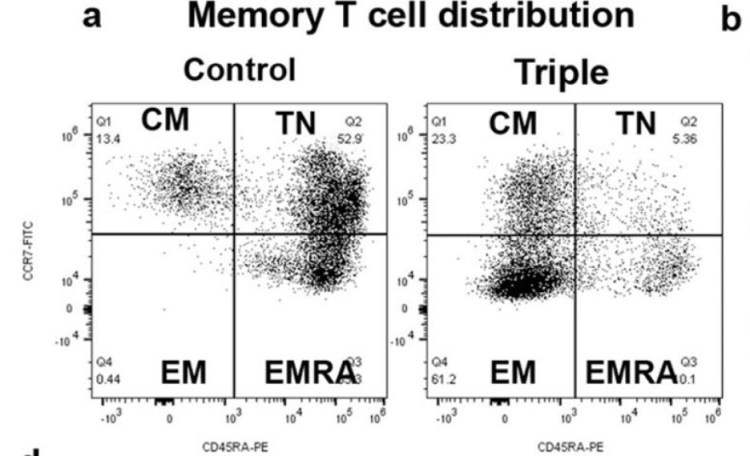
Immunoprofiling of the tumor microenvironment showed the addition of TUSC2 mediates: (a) infiltration of cytotoxic T cells, natural killer cells, and dendritic cells; (b) induction of antigen-specific T cell responses; (c) enrichment of central and memory effector T cells and (d) decreased levels of PD-1+ T cells, myeloid-derived suppressor cells, Tregs, and M2 tumor associated macrophages. Depletion studies showed the presence of functional central and memory effector T cells are required for efficacy.